Sarıçam, Ersin
Loading...

Profile URL
Name Variants
Ersin, Saricam
Saricam E.
S.,Ersin
Saricam, Ersin
Sariçam E.
E.,Sarıçam
Ersin, Sariçam
S., Ersin
E., Saricam
Sarıçam, Ersin
Ersin, Sarıçam
E.,Saricam
E., Sarıçam
Sarıçam,E.
E.,Sariçam
E., Sariçam
Sariçam, Ersin
Saricam,E.
Saricam E.
S.,Ersin
Saricam, Ersin
Sariçam E.
E.,Sarıçam
Ersin, Sariçam
S., Ersin
E., Saricam
Sarıçam, Ersin
Ersin, Sarıçam
E.,Saricam
E., Sarıçam
Sarıçam,E.
E.,Sariçam
E., Sariçam
Sariçam, Ersin
Saricam,E.
Job Title
Doçent Doktor
Email Address
ersin.saricam@atilim.edu.tr
Main Affiliation
Internal Medical Sciences
Status
Website
ORCID ID
Scopus Author ID
Turkish CoHE Profile ID
Google Scholar ID
WoS Researcher ID
Sustainable Development Goals
2
ZERO HUNGER

0
Research Products
11
SUSTAINABLE CITIES AND COMMUNITIES

0
Research Products
14
LIFE BELOW WATER

0
Research Products
6
CLEAN WATER AND SANITATION

0
Research Products
1
NO POVERTY

0
Research Products
5
GENDER EQUALITY

0
Research Products
9
INDUSTRY, INNOVATION AND INFRASTRUCTURE

0
Research Products
16
PEACE, JUSTICE AND STRONG INSTITUTIONS

0
Research Products
17
PARTNERSHIPS FOR THE GOALS

0
Research Products
15
LIFE ON LAND

0
Research Products
10
REDUCED INEQUALITIES

0
Research Products
7
AFFORDABLE AND CLEAN ENERGY

0
Research Products
8
DECENT WORK AND ECONOMIC GROWTH

0
Research Products
4
QUALITY EDUCATION

0
Research Products
12
RESPONSIBLE CONSUMPTION AND PRODUCTION

0
Research Products
3
GOOD HEALTH AND WELL-BEING

6
Research Products
13
CLIMATE ACTION

0
Research Products

Documents
26
Citations
214
h-index
7

Documents
0
Citations
0

Scholarly Output
11
Articles
11
Views / Downloads
44/0
Supervised MSc Theses
0
Supervised PhD Theses
0
WoS Citation Count
34
Scopus Citation Count
36
WoS h-index
2
Scopus h-index
2
Patents
0
Projects
0
WoS Citations per Publication
3.09
Scopus Citations per Publication
3.27
Open Access Source
7
Supervised Theses
0
Google Analytics Visitor Traffic
| Journal | Count |
|---|---|
| International Journal of General Medicine | 4 |
| Current vascular pharmacology | 1 |
| Current Vascular Pharmacology | 1 |
| Frontiers in Cardiovascular Medicine | 1 |
| Journal of health sciences and medicine (Online) | 1 |
Current Page: 1 / 2
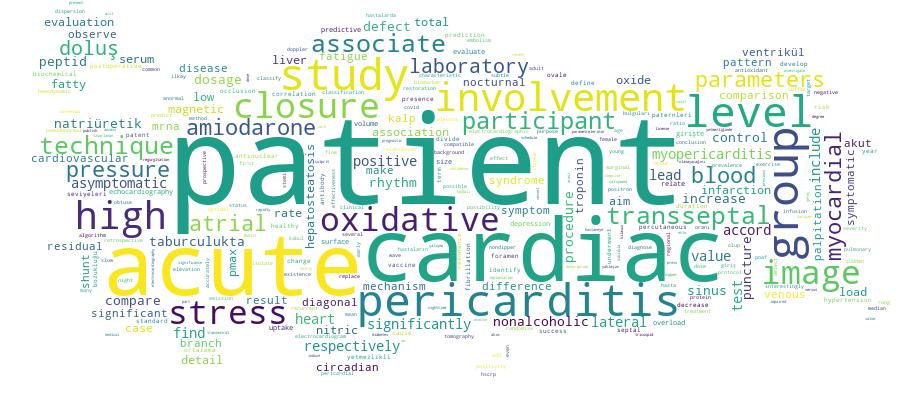
Competency Cloud